Opioid addiction is a deadly disease that’s sweeping the nation. Every day, hundreds of people die from accidental overdoses. In 2021, the U.S. experienced almost 107,000 drug overdose deaths. More than 80,000 deaths are related to opioids, and almost 88% of fatal overdoses result from synthetic opioids.
Opioids are a class of drugs that include the illegal drug heroin and pain relievers available legally by prescription, such as oxycodone, hydrocodone, codeine, morphine, and many others. Many people can take these medications without developing an addiction. However, as many as 19% of people who take legal opioid pain relievers develop an addiction. It destroys lives, families, and communities.
Suboxone® and Sublocade® are both medications medical professionals use to treat opioid dependence. Both prescription drugs contain buprenorphine, which helps reduce withdrawal symptoms and cravings. When comparing Sublocade® vs. Suboxone®, there are some critical differences between the two drugs that you should know before deciding which medication is right for you.
What is Sublocade®?
Sublocade® is a brand-name, injectable medication used to treat moderate to severe opioid addiction in people aged 18 and older. It’s a long-acting form of buprenorphine, which means it lasts for weeks or months at a time. Buprenorphine treatment may help people stop using other opioids like heroin and pain relief pills.
Sublocade® contains buprenorphine (a partial agonist), which activates the opioid receptors in your brain. This reduces the risk of over-stimulation and overdose. In clinical trials, about 30% of people who took Sublocade® for 24 weeks and had regular counseling were able to stay abstinent from opioids for 80% of the time over the course of a medication-assisted treatment plan. The placebo, which is an inactive medicine, only resulted in abstinence rates of 2% with counseling.
Sublocade®’s unique structure minimizes opioid withdrawal symptoms and cravings without producing the same “high” that other opioids do. Many people find Sublocade® is an effective treatment for opioid dependence because it makes it easier to stick to their recovery plan. A healthcare provider administers a once-monthly injection of Sublocade®. It’s a subcutaneous injection that doesn’t go into a vein. Instead, it goes under the skin.
Addiction specialists have been using Sublocade® to treat patients with opioid dependence since 2017. Sublocade® was proven more useful in clinical trials than other buprenorphine products for reducing opioid use and withdrawal symptoms.
Who Can Take Sublocade®?
Physicians only approve Sublocade®’s buprenorphine extended-release treatment for adults who have been taking other buprenorphine products, such as Suboxone®, for at least seven days. You must also be stable on your current dose of buprenorphine before you can start taking Sublocade®.
This is because Sublocade® contains a higher concentration of buprenorphine than other products. If you take Sublocade® too soon, you may experience severe withdrawal symptoms. It can also be dangerous if you take Sublocade® while you’re still using other opioids. This increases your risk of overdose.
Sublocade® treatment isn’t right for everyone. You shouldn’t take Sublocade® if you’re allergic to buprenorphine or other active ingredients in the medication. Sublocade® is also not recommended for use by pregnant or breastfeeding women or children under the age of 18. Studies are also unavailable for patients 65 or older, so Sublocade® use in this age group is not recommended. Before starting Sublocade®, tell your doctor if you’re pregnant or planning to become pregnant.
Sublocade® may interact with other daily medications you’re taking, so it’s important to tell your doctor about all the prescription medication and over-the-counter drugs, vitamins, and supplements you’re using. This includes other buprenorphine products, as well as antidepressants, antipsychotics, different opioids, and sedatives.
Sublocade® may also interact with other substances, such as alcohol. Drinking alcohol while taking Sublocade® can increase your risk of overdose and death.
How Does Sublocade® Work?
Sublocade® works by reducing withdrawal symptoms and cravings associated with opioid misuse. It does this by binding to the same brain receptors that opioids like heroin and prescription painkillers attach to. This action helps prevent the highs and lows associated with opioid use disorder.
Only healthcare professionals who have completed the training can prescribe Sublocade®. If you’re interested in Sublocade®, your first step should be to speak with your primary care or addiction specialist. A Brightside Recovery practitioner can work with you to find the right addiction treatment options. We’ll discuss the benefits and complete a Sublocade® risk evaluation before approving your treatment plan.
What Are the Risks of Sublocade®?
Sublocade® is a safe and effective medication when used as directed. However, there are some risks associated with the drug, including:
- Serotonin syndrome
- Injection site reactions
- Dizziness
- Nausea and vomiting
Some of these side effects can cause serious harm. Before starting treatment, you’ll need to discuss the risks and benefits of Sublocade® with your medical provider.
Serotonin Syndrome
Serotonin syndrome is a rare but potentially life-threatening condition that can occur when taking certain medications, including Sublocade®. This is a medical emergency if you experience any of these symptoms during your treatment.
Symptoms of serotonin syndrome include:
- Agitation
- Hallucinations
- Rapid heart rate
- High blood pressure
Anyone taking Sublocade® is at risk of serotonin syndrome, but certain people are more likely to experience this condition, including those who:
- Have a history of serotonin syndrome
- Take other medicines that increase serotonin levels in the body
- Have liver disease
- Are older than 65
These aren’t the only risk factors for serotonin syndrome. Be sure to talk to your provider regarding risks before starting medication-assisted treatment.
Injection Site Reactions
Patients receive Sublocade® injections under the skin of the upper arm, thigh, or abdomen. Some people may experience allergic reactions, including:
- Redness
- Swelling
- Itching
- Bruising
These side effects should resolve within a few days. However, contact your healthcare provider if they persist or become severe.
Is Sublocade® the Same as Suboxone®?
No. Sublocade® and Suboxone® are two different medications. Sublocade® is a monthly injection of buprenorphine, while Suboxone® is a daily film that dissolves under the tongue.
Sublocade® slowly releases into your body over the course of a month, so you don’t have to take it every day. Your physician will likely start you on a lower dose of Sublocade® and increase the dose over time. Once you reach the maintenance dose, you’ll likely stay on that single dose for the rest of the treatment.
The two drugs are used to treat opioid addiction, but they work differently. Sublocade® is best for people who are already stable on other buprenorphine products, while Suboxone® is often the first medication prescribed for opioid abuse.
While Sublocade® and Suboxone® are similar, they’re not interchangeable. Your medical provider or a clinic representative at Brightside can help you decide on the right medication treatment option for you.
Start Treatment Immediately at Brightside Recovery
Ready to start your road to recovery? Brightside offers free consultations and can help you get started right away. Through our telehealth services and medication delivery, you can do every aspect of treatment from the comfort of your home. Schedule your free telehealth consultation today to get started.
What is Suboxone®?
Suboxone® is a brand-name sublingual film used to treat opioid abuse. It’s a short-acting form of buprenorphine, which means it only lasts for a few hours at a time. It also contains naloxone, which is an opioid antagonist. Patients usually take it once or twice a day. Suboxone® is a tiny, thin sublingual film that dissolves quickly under your tongue.
It’s dispensed into four different strengths depending on the severity of the addiction. The sublingual film absorbs through the membranes of your mouth, which then enters your bloodstream faster than if you were to take it by mouth. The fast-acting nature of Suboxone® is what makes it an effective treatment for opioid addiction.
Suboxone® is an FDA-approved drug for opioid misuse. It’s also available as a generic drug. Generic drugs are usually cheaper than brand-name drugs. Suboxone® is a schedule III-controlled substance, which means it has a lower potential for abuse than other drugs in this class, which includes heroin and cocaine. The generic version is available as oral buprenorphine.
As mentioned, Suboxone® is a short-acting medication. Its effects usually last for about four hours. The half-life of a drug is how long it takes for the body to eliminate half of the drug. The half-life of Suboxone® is about 37 hours.
What Are the Side Effects of Suboxone®?
Common side effects of Suboxone® treatment include:
- Nausea
- Vomiting
- Dizziness
- Headache
Less common side effects of Suboxone® include:
- Anxiety
- Insomnia
- Rash
- Itching
- Sweating
If you experience any of these side effects, speak with a healthcare professional. They may recommend ways to ease them or adjust your dosage.
What Are the Risks of Suboxone® Treatment?
Suboxone® is a safe and effective daily medication when used as directed. However, there are some risks to be aware of. These include:
- Dependence: Suboxone® is a partial agonist, which means it can cause dependence. However, this treatment risk is lower than with different opioids.
- Withdrawal: If you suddenly stop taking Suboxone®, you may experience withdrawal symptoms. These can include nausea, vomiting, diarrhea, anxiety, and insomnia.
- Liver Damage: Suboxone® can cause liver damage, especially if you drink alcohol while taking the medication. It’s essential to avoid drinking alcohol while taking treatment containing buprenorphine.
- Pregnancy: Suboxone® may not be safe for pregnant women. If you’re pregnant or planning to become pregnant, talk to your doctor about the risks.
These are just a few of the risks associated with Suboxone®. However, these prescriptions are also effective treatments for drug dependence. If you’re considering adding Suboxone® to your treatment plan, a Brightside provider can work with you to find the best medication for your individual needs.
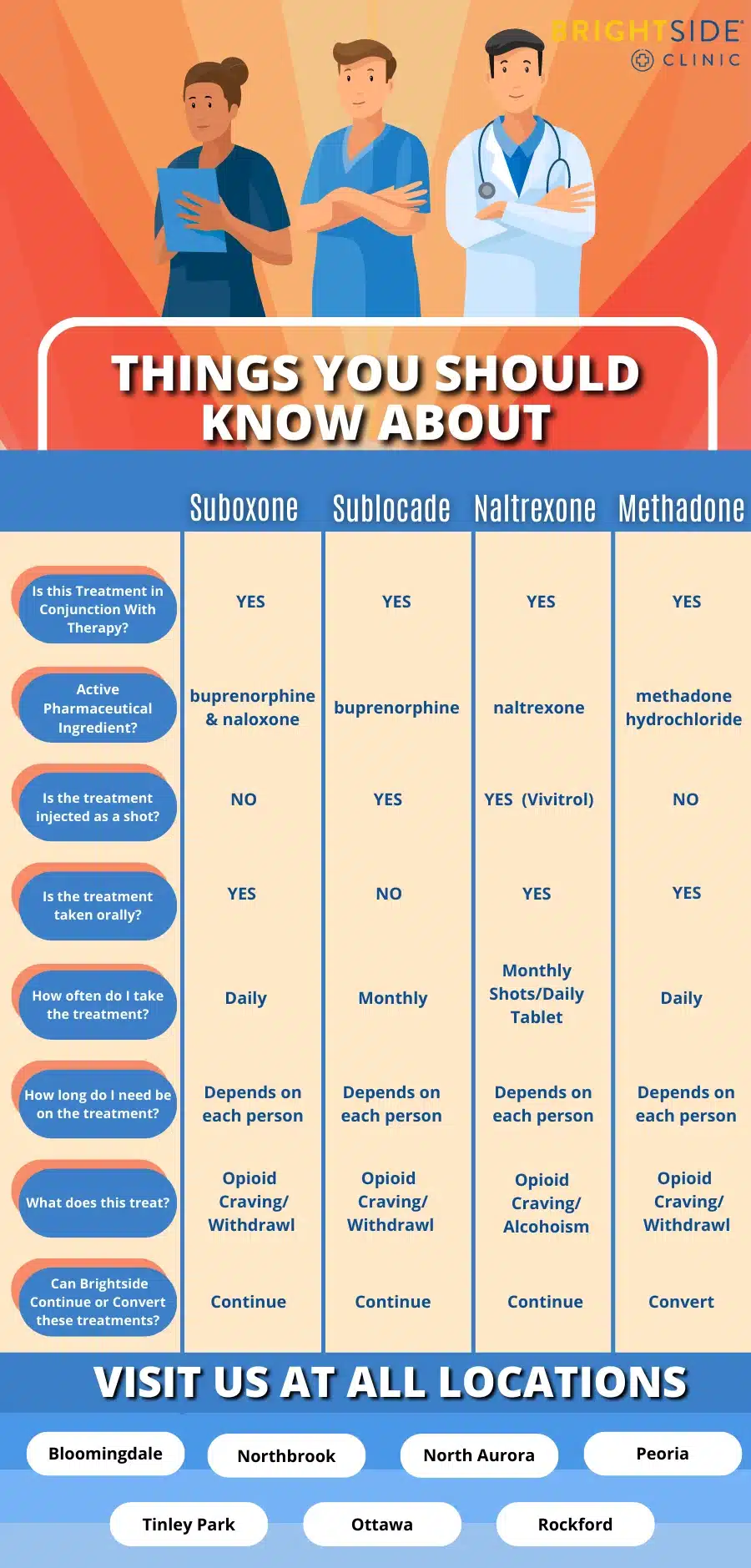
What Are the Alternatives to Suboxone® and Sublocade®?
Suboxone® and Sublocade® are just two of a few medications used to treat opiate addiction. Other common medicines include:
- Methadone
- Vivitrol/Naltrexone
- Brixadi®
These prescriptions work in different ways and have different side effects.
Choosing the Right Addiction Treatment
There are many factors to consider when choosing a treatment for opioid misuse. Working with an addiction specialist is important to find your best option.
Both Sublocade® and Suboxone® are effective treatments for opioid dependence. They work in different ways and have different side effects.
Addiction treatment depends on a few factors. Some of these include:
- The severity of your addiction: Sublocade® may be better for people with severe dependence.
- Your medical history: If you have a history of liver disease, Suboxone® may be the better choice.
- Your preferences: Some people prefer the convenience of Sublocade®, while others prefer the flexibility of Suboxone®.
- What other medications you’re taking: If you’re taking other medications, your doctor must consider drug interactions carefully.
- Your insurance coverage: Sublocade® is typically more expensive than Suboxone®.
Get the Support You Need Today
If you or someone you know is struggling with an addiction, don’t hesitate to seek help. At Brightside, we offer the help you need to get on the road to recovery. We have addiction treatment doctors available via telehealth or in locations throughout Illinois and Ohio.
Brightside Recovery offers convenient scheduling, affordable prices, and a compassionate staff that’s dedicated to helping you get your life back on track. Contact us today with your questions or to start your treatment immediately.